The war in Sudan has raged for more than 1,000 days. The fighting continues to…

Report: Covid-19 Response in Africa and the COVAX Mechanism
COVID-19 RESPONSE IN AFRICA AND THE COVAX MECHANISM
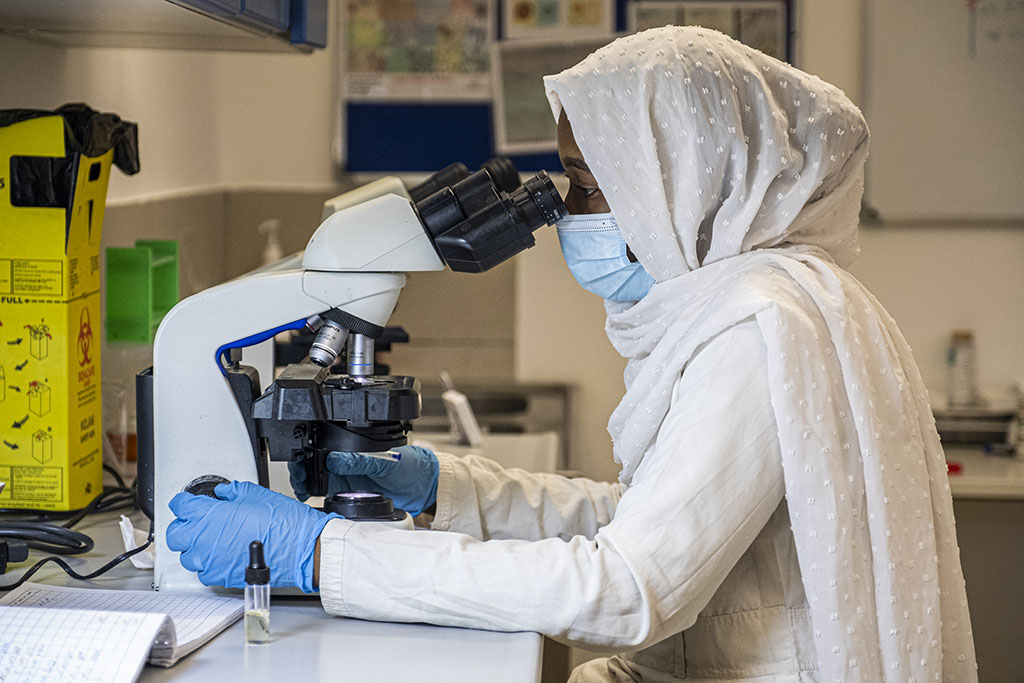
VOICES FROM THE FIELD: SIERRA LEONE, SUDAN, UGANDA
The response to the Covid-19 pandemic in Low- and Middle-Income Countries (LMICs) was largely insufficient due to global vaccine inequality and systemic issues within healthcare structures. EMERGENCY’s latest report, produced together with Bocconi University’s CERGAS and DONDENA research centres, investigates the response to Covid-19 and vaccination campaigns in three African countries: Sierra Leone, Sudan and Uganda.
The report was compiled through interviews with members of ministries of health, local health providers, staff and technicians from international organisations, and staff from EMERGENCY’s hospitals in Goderich, Khartoum and Entebbe; it concludes with key recommendations to ensure proper preparation for, and an equitable response to, the inevitable next global pandemic.
Background
The Covid-19 pandemic strained the world’s health systems, particularly those in LMICs. It disrupted routine immunisations, diagnosis and treatment of diseases, maternal and child healthcare, and other health services.
The initial economic impact in African countries was severe, pushing tens of millions more people into extreme poverty (World Bank), while containment efforts prompted long school closures and disrupted global supply chains, intensifying food insecurity.

African governments have obtained Covid-19 vaccines through direct purchases, bilateral donations, and the multilateral COVAX initiative—an international effort to provide quick and equitable vaccine access to the world’s most vulnerable, regardless of a country’s ability to pay. The COVAX mechanism continues to be the leading source of vaccines delivered to Africa, accounting for more than 60% of doses received (Africa CDC).
As of March 2023, around 2 billion vaccine doses had been shipped to 146 recipient countries through the COVAX mechanism (UNICEF). However, the goal of vaccinating at least 70% of each country’s population by mid-2022 has fallen far short (WHO); in Africa, only 36% of people have received at least one dose (Johns Hopkins).
Sierra Leone, Sudan and Uganda
African countries generally lack the facilities and infrastructure required to produce, transport and store the Covid-19 vaccines. Among the world’s poorest countries, they were also unable to compete with wealthier countries to purchase doses. Together, these constrained distribution and administration activities.
While each country’s response was slightly different – Sierra Leone, in particular, drew on its experience dealing with the Ebola epidemic – there are common needs to be addressed.

Health Workers. The World Health Organization has set a standard of 4.45 health workers per 1,000 people. Sierra Leone has 0.82 health workers per 1,000 people; Sudan, 1.41; and Uganda, 1.79. The vast majority of these health workers are nurses. Inadequate funding and neglect for health workers’ safety (such as limited provision of PPE), on top of already-inadequate levels of health workers, led to disruptions in regular healthcare services and limited the effectiveness of the countries’ Covid-19 responses.
Communication. Mismatches between international and national media channels, and between national and informal media channels, generated further vaccine hesitancy. General distrust in the government, particularly in Sudan, encouraged conspiracy theories and impeded the distribution of vaccines. Governments failed to target messaging or address the concerns of different segments of the population; low symptomatic rates and adults’ expectations that vaccinations are for children were particularly challenging obstacles.
Vaccine Roll-out. While each country’s government eventually established an adequate vaccination campaign, national difficulties with data collection and reporting makes it difficult to assess true rates of infection and vaccination. The reliance of the three countries on external aid was exacerbated by the pandemic response; with no internal vaccine production capabilities, they were entirely dependent on the international community, with the subsequent delivery of vaccines delayed and incomplete (hundreds of millions of promised doses were never delivered). Of the vaccines that were delivered, many went to waste because of their short shelf-life, inadequate for countries with limited roll-out capacities.
Key Recommendations
The report concludes with 11 key recommendations, including a call for inclusive global policy-making that would contextualise issues and responses; broaden external aid to include capacity-building rather than just resource allocation, particularly focusing on local health workforces to achieve the WHO threshold of 4.45 health workers per 1,000 people; and increase public health knowledge and institutional trust to increase the effectiveness of emergency response measures.
Diseases know no borders; we must increase global readiness to prepare for and mitigate the next global health threat.



